Multiple persistent infections: Difference between revisions
| Line 138: | Line 138: | ||
=== Triple antibiotic combination (Daptomycin + Cefoperazone / Cefuroxime + Doxycycline) === | === Triple antibiotic combination (Daptomycin + Cefoperazone / Cefuroxime + Doxycycline) === | ||
Zhang and colleagues | Zhang and colleagues had previously studied the effect of antibiotic combinations on Borrelia persisters (https://doi.org/10.3389/fmicb.2016.01744). They found that a triple combination of antibiotics was effective in laboratory situations. This antibiotic combination has yet to be studied in lab animals or humans. | ||
One of Zhang's students, Megan Weitner, wrote her 2016 thesis | One of Zhang's students, Megan Weitner, wrote her [[Megan_weitner%27s_2016_thesis|2016 thesis]] on drug combinations that had effectiveness against Borrelia in lab settings. They include artemisinin, nitrofurantoin, azithromycin, methylene blue, doxycycline, hydroxychloroquine, and rifabutin. | ||
=== Polyphenolic compound combination === | === Polyphenolic compound combination === | ||
Revision as of 03:26, 27 May 2022
Introduction
What's old is new again. Long haul syndromes (long COVID and vaccine injury) can be thought of as variations on chronic health conditions that have previously existed. The symptoms of long haul overlap the symptoms of ME/CFS, breast implant illness, Gulf War Syndrome, post viral syndromes (polio, MERS, Ebola, etc.), chronic Lyme, Essure injury, POTS, dysautonomia, etc.
ME/CFS versus post vaccination syndrome symptoms are compared below:
Data from:
- https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2429637/pdf/postmedj00163-0031.pdf
- https://www.react19.org/post/persistent-neurological-symptoms-patient-survey
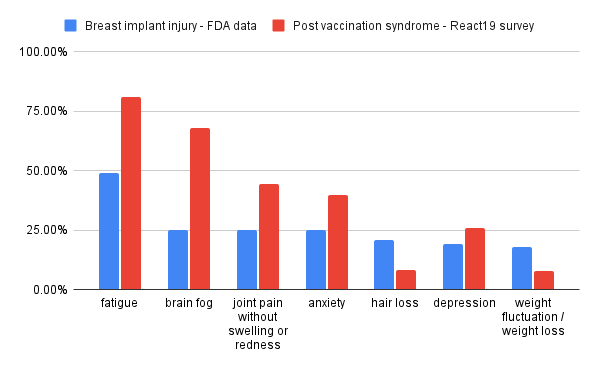
Breast implant illness versus post vaccination symptoms are compared below:
Data from:
- https://www.fda.gov/medical-devices/breast-implants/medical-device-reports-systemic-symptoms-women-breast-implants
- https://www.react19.org/post/persistent-neurological-symptoms-patient-survey
The common denominator
The common thread that runs through long haul, ME/CFS, and breast implant illness (BII) are infectious diseases. Breast implants, while being inorganic and biologically inactive, turn out to be an excellent environment for bacteria and fungi. One observational study on BII patients found that BII patients were six times more likely to have culturable bacteria or fungi/yeast growing on their implants compared to healthy controls.
ME/CFS is also a condition that has been linked to infectious diseases:
- Various infectious diseases: enteroviruses, herpesviruses including Epstein-Barr virus, Q fever, coxsackie b, and Ross River virus.
- Outbreaks
- Stress, e.g. from a divorce. Stress is thought to weaken the immune system.
- Trauma, e.g. a car accident, head injury, etc.
The data suggests that many different paths can lead to the body being unable to control persistent infections.
The diversity of the bacteria, viruses, yeast, parasites, etc. that live inside humans would explain why symptoms vary so much from patient to patient. Various chronic illnesses may all be different facets of a similar underlying problem: persistent infections that the immune system is unable to contain.
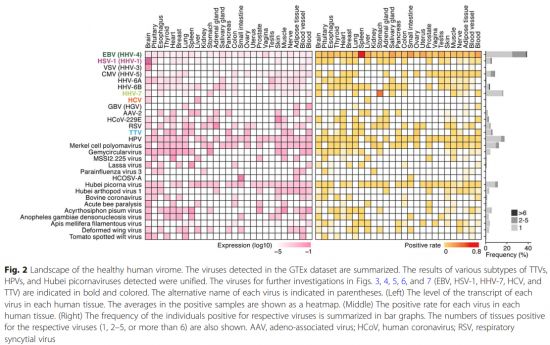
The healthy human virome
Kumata and colleagues published the paper A tissue level atlas of the healthy human virome (https://doi.org/10.1186/s12915-020-00785-5). Their study examined the various viruses that live inside health human beings. One of their findings was that viruses don't always live in the same places in the body. One person might have Epstein-Barr virus (EBV) living only in their spleen while another person might have EBV living in multiple organs.
One phenomenon seen in a few long haulers are reactivated infections. Pre-existing viruses such as EBV, shingles / herpes zoster / varicella-zoster virus, etc. turn into more active infections and can be detected in the blood using commercially available tests. This suggests that the immune system is dysfunctional and unable to suppress persistent infections like a healthy immune system would.
The natural variations in the types of microorganisms living in a person and where they reside may explain why there are so many different symptoms and why they vary so much from person to person. A survey of long COVID patients published in The Lancet (https://doi.org/10.1016/j.eclinm.2021.101019) analyzed 203 (!!) different symptoms in long COVID sufferers.
Successive infection ("teamwork makes the dream work")
Microorganisms sometimes fight each other, e.g. by producing toxic poisons such as penicillin to kill off competing species fighting for the same resources. However, it is also possible for microorganisms to act synergistically in suppressing the immune system. All microorganisms living in humans tend to be able to do so because evading the immune system is typically essential for their survival.
Proal and colleagues (https://doi.org/10.1097/BOR.0b013e32835cedbf) discuss how Epstein-Barr Virus, Borrelia (Lyme), CMV, and other microorganisms all interfere with the immune system by dysregulating the vitamin D receptor pathway. Their paper argues that a greater number of pathogens in the microbiome contributes to greater dysfunction in the immune system, eventually leading to chronic illness. Amy Proal explains these concepts in a Youtube video (https://youtu.be/7yjh04vMe1E).
It is also known that the HIV virus synergizes with other microorganisms (e.g. JC virus, the fungus pneumocystis jirovecii) in killing its host.
Auto-immunity
Auto-antibodies are antibodies that engage in 'friendly fire' and stick to the host's proteins/antigens instead of the foreign antigens associated with pathogens. A study by Gerd Wallukat and his team on recovered COVID-19 patients (https://doi.org/10.1016/j.jtauto.2021.100100) found that all had between 2 and 7 different auto-antibodies of the GPCR-fAAB type (g-protein coupled receptor functionally active auto-antibodies). In healthy controls, such auto-antibodies are only found in a small percentage of people.
Proal and colleagues (https://doi.org/10.1097/BOR.0b013e32835cedbf) believe that such autoimmunity processes are being driven by molecular mimicry, a defense strategy where microorganisms evolve their external antigens to be extremely similar to the host's antigens. This strategy makes it difficult for the immune system to attack problematic microorganisms without also attacking host tissue.
While many autoimmune conditions are treated by suppressing the immune system and reducing the amount of 'friendly fire' from the immune system, such a strategy does not deal with the root cause: persistent infection. This may explain why immune suppression strategies (e.g. corticosteroids) fail in some/many patients. The patient's immune system is already unable to contain persistent infections and further suppression of the immune system only makes the underlying problem worse.
Autoimmunity seems to be quite common following knee replacement surgery. A prospective case-control study of 796 TKA patients (https://doi.org/10.1111/os.12934) found that 20.35% (162/796) of the patients developed subclinical hypothyroidism with anti-TPO auto-antibodies.
A paper by Warkentin and Greinacher (https://www.sciencedirect.com/science/article/pii/S0049384821003571#bb0505) argues that knee replacement leads to a blood-clotting syndrome (spontaneous heparin-induced thrombocytopenia) that is very similar to vaccine-induced immune thrombotic thrombocytopenia. Whereas heparin-induced thrombocytopenia (HIT) can develop following exposure to heparin, the authors believe that HIT can develop without exposure to heparin. They refer to that form of HIT as spontaneous HIT. In knee replacement patients, around 26% (!) develop auto-antibodies against PF4. While the authors do not point out a common autoimmunity-generating mechanism between vaccination and knee replacement surgery, it is known that infections (such as coagulase-positive S. Aureus) commonly form biofilm colonies on foreign objects inside the body. The inability to suppress S. Aureus or other infections in the body could explain why clotting disorders are quite common in knee replacement patients and are occasionally seen in the vaccine injured.
Current treatments
Unfortunately, it is difficult to treat persistent infections because the tests usually miss the infection and the treatments are often ineffective. Most microorganisms are extremely difficult or impossible to detect in the blood because they do not live in the blood and are quickly wiped out by the immune system if they make their way into the bloodstream. Research on the Lyme-causing bacteria Borrelia Burgdorferi by Monica Embers and her team has found that invasive, research-level tests are usually needed to detect persistent Borrelia infections (https://doi.org/10.3389/fmed.2021.666554). Her team also found that standard antibiotic treatments do not work since the Borrelia Burgdorferi bacteria form biofilm colonies that are incredibly resistant against the immune system and antibiotics.
Antibiotics
The 2014 ILADS treatment guidelines recommends the use of antibiotics in treating cases of chronic Lyme:
ILADS recommends antibiotic retreatment when a chronic Lyme infection is judged to be a possible cause of the ongoing manifestations and the patient has an impaired quality of life
Antiparasitics
Various antiparasitic drugs such as ivermectin have good safety profiles and are highly effective against parasites. Ivermectin has demonstrated effectiveness in treating SARS-CoV-2 coronavirus infections; see ivmmeta.com for a list of studies and Lawrie and colleagues for a meta-analysis. Ivermectin is part of the FLCCC I-RECOVER protocol for the treatment of long COVID (PASC) and vaccine injury (post vaccination syndrome).
Toxoplasma prevalence and treatment
Toxo is a common parasitic infection, with 15.8% of the US population having positive antibody tests against the parasite (https://dx.doi.org/10.3201/eid0911.030098). The US CDC notes that toxo "can be treated with a combination of drugs such as pyrimethamine and sulfadiazine, plus folinic acid".
Antifungals
Various antifungal drugs are effective against such fungal infections. However, fungi microorganisms that pursue a biofilm colony growth strategy are incredibly resistant against antifungal drugs.
Antivirals
Many viral diseases do not have a treatment. Some exceptions include:
- Herpes zoster (shingles): Acyclovir (Zovirax), Famciclovir, Valacyclovir (Valtrex)
- HIV: antiretrovirals
- Hepatitis C: Ledipasvir/Sofosbuvir (Harvoni), Simeprevir (Olysio), etc.
Interferon drugs
Interferons are molecules produced by the body's cells that "interfere" with the reproduction of viruses, hence the name interferon. There are many types of interferons. The pharmaceutical has developed interferons that are modified with polyethylene glycol (PEG); these are called pegylated interferons.
Interferons can be introduced into the body to help fight viral infections. However, interferon drugs alone are often not enough to cure hepatitis C. Both pegylated and non-pegylated interferons are used to treat both viral infections (e.g. hepatitis C) and autoimmune diseases (e.g. Rebif / interferon beta-1a is used to treat multiple sclerosis). Ironically, peginterferon alfa-2a seems to increase the chances of a new autoimmune disease developing in the patient.
Interferon-inducing drugs
Former Soviet Bloc countries (e.g. Russia, Ukraine) use interferon-inducing drugs such as tilorone to treat viral infections and multiple sclerosis, an autoimmune disease. Tilorone is low-cost, widely used, and is sold over the counter.
Removal of foreign objects from the body
Bacterial and fungus biofilms are known to grow on breast implants and replacement joints, possibly facilitated by the inorganic/abiotic nature of these objects' surfaces or the body's formation of scar tissue around them. Complete removal of breast implants tends to have excellent outcomes, with most patients seeing significant improvement in their chronic health issues following explantation. Other objects are difficult to remove safely (e.g. pacemakers, replacement heart valves) or are difficult to remove completely (e.g. mesh, Essure), leading to less impressive improvements in chronic health issues following surgery.
This area of medicine provides the strongest evidence that infections are the root cause of chronic health problems and autoimmune conditions. The study by Lee and colleagues (https://dx.doi.org/10.1097%2FGOX.0000000000002755) found that 14 out of 15 patients with a post-implant autoimmune condition saw their autoimmune condition improve or resolve.
For more information, see the page on foreign object infections.
Potential / experimental treatments
Essential oils, carvacrol, and cinnamaldehyde
Feng, Zhang and colleagues studied the effect of various essential oils on Borrelia bacteria living in biofilms in their 'persister' form (https://doi.org/10.3390/antibiotics7040089). They found that antibiotics were mostly ineffective at stopping the bacteria and that certain essential oils were more effective than antibiotics at killing the bacteria. They also identified that the chemicals carvacrol and cinnamaldehyde, major components of effective essential oils, are potent chemicals against Borrelia persisters. Their findings have yet to be tested in human beings and these chemicals may not necessarily be effective in treating Borrelia infections in humans.
Carvacrol-containing supplements that are commercially available include black seed oil (from the nigella sativa plant) and oil of oregano. One brand of black seed oil (Maju Superfoods) contains instructions that call for 4 teaspoons per day, suggesting that such a dosage may be safe for human consumption. 1-star reviews on Amazon and iHerb provide some information on what can go wrong with this type of supplement.
Cinnamaldehyde can be ingested through toothpicks infused with cinnamon oil. Sucking on such toothpicks is part of the local food practices in some areas of the United States. 1-star reviews on Amazon suggests that these toothpicks can cause mouth sores in some people.
Warning: Some essential oils cause chemical burns, especially if undiluted. Some cause photosensitivity (tendency to become sunburned) if they are ingested or applied to the skin. The Now Foods website has a FAQ on ingesting essential oils that you should read before doing anything stupid. A webpage on essential oil toxicity notes that volumes "of 5-15mL are likely to cause toxicity in adults". That threshold may be dramatically lower for cinnamon oil and tea tree oil, which have significantly lower LD50 values than other essential oils. (LD50 refers to the Lethal Dose needed to kill 50% of lab animals.) Here are LD50 values for some essential oils:
- Orange essential oil: >5000 mg/kg (source)
- Lavender essential oil: 4000 - 10000 mg/kg (source)
- Cinnamaldehyde, a major component of cinnamon essential oil: 2.22 mg/kg (source)
- Tea tree oil: 1.7 mg/kg (source)
Tea tree oil (Melaleuca alternifolia)
While tea tree oil causes chemical burns in humans, it may be effective in humans at low doses. When tested in cell cultures, tea tree oil has demonstrated antimicrobial action against a wide range of microorganisms (https://dx.doi.org/10.1155/2016/3012462):
Alternaria spp. A. flavus, A. fumigates, A. niger, Blastoschizomyces Capitatus, C. albicans, C. glabrata, C. parapsilosis, C. tropicalis, Cladosporium spp., C. neoformans, Epidermophyton floccosum, Fusarium spp., Malassezia furfur, Microsporum canis, M. sympodialis, M. gypseum, Penicillium spp., Rhodotorula rubra, Saccharomyces cerevisiae, Trichophyton mentagrophytes, T. rubrum, T. tonsurans, Trichosporon spp.
One commercially-available supplement that contains tea tree oil is Biocidin. Amazon reviews suggest that the product works, although the negative reviews note serious side effects:
The die off on this product caused me to be bed bound for over 3 months. The doctor who suggested I take it did not know the consequences. It caused major enormous skin eruptions on several parts of my body and took several months to heal. My doctors took me off it because of the die off since he did not know it would cause so much pain and suffering. I could not walk or get out of bed. Be very very careful.
Triple antibiotic combination (Daptomycin + Cefoperazone / Cefuroxime + Doxycycline)
Zhang and colleagues had previously studied the effect of antibiotic combinations on Borrelia persisters (https://doi.org/10.3389/fmicb.2016.01744). They found that a triple combination of antibiotics was effective in laboratory situations. This antibiotic combination has yet to be studied in lab animals or humans.
One of Zhang's students, Megan Weitner, wrote her 2016 thesis on drug combinations that had effectiveness against Borrelia in lab settings. They include artemisinin, nitrofurantoin, azithromycin, methylene blue, doxycycline, hydroxychloroquine, and rifabutin.
Polyphenolic compound combination
Anna Goc and colleagues studied a combination of six plant-based compounds in both mice and humans (https://doi.org/10.1177/2040622320922005):
- Baicalein
- Luteolin
- Rosmarinic acid
- The fatty acids monolaurin and cis-2-decenoic acid
- Iodine/kelp
When trialed on human patients suffering from chronic Lyme, the results were:
- 3/17 symptom free
- 8/17 significant improvement
- 2/17 slight improvement
- 4/17 no improvement, minor side effects from treatment (that resolved after treatment was stopped)
There was no control group in the trial, so it is not entirely clear if the drug combination would have outperformed a placebo treatment. The compounds were purchased from specialty suppliers to achieve higher purity than the same compounds available from mass-market consumer-grade supplements.
Olmesartan
Olmesartan is a repurposed drug being used experimentally to treat chronic illness. Proal and colleague's 2011 paper Immunostimulation in the era of the metagenome (https://doi.org/10.1038/cmi.2010.77) describes their experiences with using the drug to stimulate the immune system via the vitamin D receptor. Their paper describes both positive and negative results, sometimes after years of treatment.
Remdesivir
The World Health Organization does not recommend the use of remdesivir for the treatment of SARS-CoV-2 (the virus that causes COVID). However, a ME/CFS specialist named John Chia is trying the drug as a way to treat enterovirus infections (see this interview with Chia).
During the French 'DisCoVeRy' trial, 1-3 patient deaths were attributed to remdesivir. According to the paper on the clinical trial results:
Three deaths (acute respiratory distress syndrome, bacterial infection, and hepatorenal syndrome) were considered related to remdesivir by the investigators, but only one by the sponsor's safety team (hepatorenal syndrome).
Meat-only diet and elimination diets
Survey data on those consuming a 'carnivore' diet suggests that diet can cure or improve autoimmune conditions. Other elimination diets also show effectiveness against autoimmunity, but with less spectacular results. Randomized controlled trials have shown that elimination diets are effective in improving outcomes in rheumatoid arthritis patients. See the page on meat-only elimination diets for summaries of research on the effect of diet on autoimmunity.
Those consuming a carnivore diet often report that they no longer catch the common cold, possibly suggesting that the diet resolves autoimmunity by boosting the immune system. Another possibility is intestinal permeability or 'leaky gut'. Meat-only diets help restore intestinal permeability, possibly restricting the passage of foreign antigens and/or pathogens into the bloodstream. Vieira and colleagues (https://doi.org/10.1126/science.aar7201) have demonstrated that a gut microorganism drives autoimmunity in mice and humans by translocating into the body.
Disclaimer
Successive infection is a theory popularized by Amy Proal, Michael VanElzakker, and their colleagues in papers such as Autoimmune disease in the era of the metagenome (https://doi.org/10.1016/j.autrev.2009.02.016) and Youtube videos such as their interview with Steven Phillips and Dana Parish (https://youtu.be/cYo32Qd5ncI). Steven Phillips has also made multiple appearances on Dr. Been's Youtube channel (on chronic disease, long COVID, and dementia) where he talked about how infections cause autoimmune disease and chronic health problems.
Their views challenge mainstream medicine's views on autoimmunity and are not currently part of the medical establishment's scientific consensus. The limitations of current medical testing and treatments make these theories difficult to prove and to translate into cured patients, except in patients where foreign objects can be safely removed. Both Amy Proal and Steven Phillips were bedridden for around two years before their health turned around.