Foreign object infections
Breast Implant Illness[edit]
Scientific research suggests that non-organic/abiotic objects in the human body create a fertile environment for bacterial and fungal biofilms, which can cause chronic illness. For people with breast implants, removing this environment from the body often (but not always) leads to significant improvement in chronic health issues.
It is currently unclear why a small portion of human beings do not tolerate inorganic objects inside their bodies, especially given that some healthy people do not show symptoms even though they have biofilms growing on their implant or prosthetic. One possibility is that the microorganisms in the body become imbalanced and synergistically support each other in suppressing the immune system ("successive infection"), resulting in a state where the immune system can no longer suppress persistent infections.
Introduction[edit]
FDA data shows that chronic health problems are reduced in most patients who decide to have their breast implants removed (explantation). Nonetheless, breast implant illness (BII) is a controversial illness as many doctors do not believe that breast implants can lead to the development of chronic health problems. Despite presenting data on health outcomes following explantation, the FDA notes that "BII is not recognized as a formal medical diagnosis". BII occurs across all implant types, textured and untextured, as well as damaged and undamaged.
There is currently no test to detect BII and no test that can help predict the outcome of explantation. However, medical tests can find other reasons to explant such as a damaged implant.
One theory is that the bacterial biofilm colonies growing on breast implants are responsible for chronic health issues. A study by Lee and colleagues found that culturable bacteria and other microorganisms were 6 times more common in BII patients than non-BII patients with breast implants.
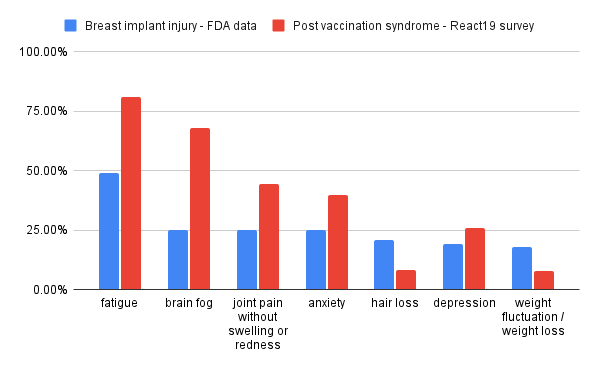
Overlap between BII and post-vax long haul[edit]
Both BII and vaccine injury show a significant overlap in symptoms. Whereas many vaccine injury and long COVID patients see a significant improvement in symptoms after several months, BII does not seem to exhibit a similar pattern. It is unclear if BII and long haul are two different facets of a similar process, or if they are distinct illnesses.
Because there is currently no test to differentiate between BII and long haul (aside from time), both patients and their doctors should consider the possibility of BII.
Symptom data from:
- https://www.fda.gov/medical-devices/breast-implants/medical-device-reports-systemic-symptoms-women-breast-implants
- https://www.react19.org/post/persistent-neurological-symptoms-patient-survey
Published case studies have also noted adverse reactions with implants following vaccination:
- Potential immune response to breast implants after immunization with COVID-19 vaccines https://dx.doi.org/10.1016/j.breast.2021.06.002 - Case series on 4 patients
- Breast implant seroma: A SARS-CoV-2 mRNA vaccine side effect https://doi.org/10.1002/jcu.23056 - Case study
- A Case Report of Capsular Contracture Immediately Following COVID-19 Vaccination https://doi.org/10.1093/asjof/ojab021
VAERS contains reports of breast implant reactions following vaccination:
- 2041984 - implants became infected, one implant was removed
- 2041988 - device related infection
- 2110504 and 2110516 - "left breast implant felt hard. It was swollen and it was very painful"
- 2175343 - "her left saline implant looked like a cow's nipple, breasts are like cow nipple, ruined chest"
- 2179427 - "She reports lots of pain in her left arm where she got it; The whole breast on the left side was swollen."; Yesterday she found a "huge lump" in her left breast;"
- 2252550 - "tenderness at breast implants"
FDA data[edit]
Outcomes[edit]
Of the 3,577 MDRs [Medical Device Reporting reports], 1535 (or 43%) reported the patient undergoing device explant at some time following the onset of symptoms. Of these, 1,473 reports provided information sufficient to calculate the time from implantation to explant. The average time to explant was 9 years, with a range of 0- 47 years. Only 290 MDRs provided information related to the status of a woman’s symptoms following explant. Of these, 279 noted improvement and 11 noted either no improvement or worsening of symptoms.
Most common systemic signs or symptoms[edit]
| Symptom | Percentage of MDRs (N=3,577) |
|---|---|
| Fatigue | 49% |
| "Brain Fog" | 25% |
| Joint Pain | 25% |
| Anxiety | 24% |
| Hair Loss | 21% |
| Depression | 19% |
| Rash | 18% |
| Autoimmune Diseases (incl. symptoms of autoimmune disease) | 18% |
| Inflammation | 18% |
| Weight Fluctuation | 18% |
Data on explantation outcomes[edit]
- FDA data: https://www.fda.gov/medical-devices/breast-implants/medical-device-reports-systemic-symptoms-women-breast-implants
- 87.7% (577/657) of women noted an improvement in symptoms following explant, with the rest noting either no improvement or worsening of symptoms.
- NIH data: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8342259/
- 23% of patients reported complete resolution of symptoms following explantation, with 74% reporting partial resolution. Only 3% reported no improvement.
- Glicksman and colleagues: https://doi.org/10.1093/asj/sjad098
- At one year, 88% of patients showed at least partial symptom improvement with a reduction of 2-20 symptoms.
- Systemic symptom improvement was noted out to one year in the BII Cohort regardless of the type of capsulectomy performed.
- Lee and colleagues: https://doi.org/10.1097/GOX.0000000000002755
- 84% of patients reported partial or complete resolution of BII symptoms on Patient-Reported Outcome Questionnaire.
- 14/15 patients reported "Postoperative Improvement or Resolution" of their autoimmune diagnosis
- Serena et al.: https://doi.org/10.7759/cureus.38056
- Retrospective survey design with patients dropping out of the study (weak design)
- Results: "The study achieved a total of 549-point decrease in symptom frequencies following surgery. Furthermore, with an average preoperative symptom score of 3.5 (scored 1-5) and a postoperative average of 1.9, the study demonstrated a score reduction of 1.6 across all symptoms. Furthermore, the study was able to eliminate on average 2.8 symptoms of breast implant illness from every patient following explantation."
Outcomes in long haulers[edit]
See slides 31-32 from a presentation on experimental treatment of vaccine injury (slides, video). 1 Long COVID sufferer reported an improvement. Among 2 vaccine injured patients, one reported no difference while the other reported some improvement (following significant initial worsening).
Warning: Long haulers may tolerate surgery less than healthy individuals[edit]
Anecdotal evidence suggests that long haulers suffer more adverse events from surgery than health individuals. It is currently unclear if there may be additional risk that would change the risk/benefit of surgery.
Scientific papers[edit]
- ‘ASIA’ – Autoimmune/inflammatory syndrome induced by adjuvants https://www.sciencedirect.com/science/article/abs/pii/S0896841110000788 - This review paper (over 800 citations) discusses how autoimmune syndromes are linked to vaccine adjuvants, breast implants, and Gulf war syndrome (GWS).
- Autoimmune dysautonomia in women with silicone breast implants https://doi.org/10.1016/j.jaut.2021.102631 - The authors discuss a correlation between auto-antibodies and symptom severity, suggesting that autoimmunity is the cause of symptoms. It is unclear if auto-antibody tests may be useful in diagnosing BII or predicting explantation outcomes.
- Breast Implant Illness: A Biofilm Hypothesis https://dx.doi.org/10.1097%2FGOX.0000000000002755
- Still's disease, lupus-like syndrome, and silicone breast implants. A case of 'ASIA'(Shoenfeld's syndrome) https://www.researchgate.net/profile/Miguel-Saavedra-13/publication/221738376_Still%27s_disease_lupus-like_syndrome_and_silicone_breast_implants_A_case_of_%27ASIA%27_Shoenfeld%27s_syndrome/links/0a85e5325f08a081a5000000/Stills-disease-lupus-like-syndrome-and-silicone-breast-implants-A-case-of-ASIA-Shoenfelds-syndrome.pdf
- Two hundreds cases of ASIA syndrome following silicone implants: a comparative study of 30 years and a review of current literature https://doi.org/10.1007/s12026-016-8821-y
- Chronic fatigue syndrome with autoantibodies—the result of an augmented adjuvant effect of hepatitis-B vaccine and silicone implant http://www.cfsitalia.it/Documenti/ChronicFatigue_HBV_vaccine_silicone_implants.pdf - This case report suggests that there are safety concerns with giving vaccines (specifically Hepatitis B) to individuals with silicone implants.
- Silicone Gel Breast Implants and Connective Tissue Disease—A Comprehensive Review https://sci-hub.se/https://doi.org/10.1080/08916931000148818 - Discusses the correlation between breast implants and scleroderma, a group of rare diseases that involve the hardening and tightening of the skin. Scleroderma is believed to be an autoimmune disease.
The scientific literature refers to BII as siliconosis, ASIA / autoimmune/inflammatory syndrome induced by adjuvants, and silicone implant incompatibility syndrome. Many articles on this topic can be found by searching Google Scholar.
Parallels between BII and replacement joint infections[edit]
The scientific literature strongly suggests that both conditions are caused by similar processes. With breast implants, the study by Lee and colleagues (https://dx.doi.org/10.1097%2FGOX.0000000000002755) found that Propionibacterium acnes, Staphylococcus epidermidis, and fungal Candida species all grow on implants. All of those species have also been found growing on prosthetic/replacement joints.
- A joint infection study by Achermann and colleagues (https://dx.doi.org/10.1128%2FJCM.00006-10) have found Staphylococcus aureus, Coagulase-negative staphylococci, Streptococcus species (mitis, agalactiae, dysgalactiae, gallolyticus, pneumoniae), Propionibacterium acnes, and Candida albicans.
- Koskela and colleagues (https://doi.org/10.1007/s10096-008-0664-6) as well as Hischebeth and colleagues (https://doi.org/10.1016/j.diagmicrobio.2018.08.012) discuss the role of Staphylococcus epidermidis in replacement joint infections.
Despite the parallels, a BII diagnosis is not mainstream while a joint infection diagnosis is mainstream. Both sets of literature rarely reference one another.
In terms of detecting infections growing on foreign objects, the replacement joint literature rarely recognizes the difficulties associated with detecting microorganisms. There is a presumption that their medical tests have very few false positives and false negatives. There is very little discussion about patients who may be suffering because they have an infection that is difficult to detect. The microbiology literature has plenty of information on microorganisms that are difficult to detect. Many microorganisms have a "viable but non-culturable" state where they are living but not dividing; usually microorganisms enter this state to survive harsh environments until more favourable conditions arrive that would allow them to reproduce and flourish (see https://doi.org/10.1016/j.mimet.2011.04.018). For many species, scientists do not know how to get these microorganisms to replicate. Some areas of medicine wrongly assume that there is no infection because the lab is unable to culture the microorganisms and get them to reproduce. This may potentially cause many chronic conditions to be underdiagnosed. In the BII study by Lee and colleagues (https://dx.doi.org/10.1097%2FGOX.0000000000002755), only 36% of the breast implants were associated with a positive culture test while 84% of the explantation surgeries led to improvements in symptoms. This suggests that culture tests (even with better methodology such as sonication) would miss most patients who would benefit from explantation.
With breast implant illness, many doctors do not believe that such a condition exists so their denial may be the leading cause of underdiagnosis.
Support groups[edit]
Support groups and communities can be found via Facebook and Youtube (search Youtube for "breast implant illness"). The largest Facebook support group is Breast Implant Illness and Healing by Nicole with 159k members.
They may share information on how to find doctors who are knowledgeable about BII.
Support groups may have certain biases such:
- The viewpoint that the capsule scar tissue is also a cause of BII and should be removed during explantation.
- Favoring explantation.
More resources[edit]
Breast Implant Illness .com has a wealth of information on symptoms, tests, surgeons, etc.
[edit]
Introduction[edit]
The dominant narrative in the literature for joint replacements and medical devices is that bacterial and fungal biofilms are responsible for infections that lead to chronic health problems.
Overlap between orthopedic implants and vaccination[edit]
A case study series by Elkousy and colleagues (https://doi.org/10.1016/j.xrrt.2021.12.003) notes that adverse events following mRNA vaccine administration were observed in their orthopedic practice's patients. One of the four patients also had a reactivated herpes zosters (shingles) infection, suggesting that vaccination disrupted the normal functioning of the patient's immune system.
VAERS contains one or more reports of joint replacement interactions following vaccination:
- 2107567 - "½ cup of blood was removed from knee joint in ER; diagnosis that she had fluid in her knee; On Sunday 27Mar2021, three of her joints swelled and caused her pain. All three joints were the subject a joint replacement at some point in the past. "
Dental implants and long COVID[edit]
A case study series described by Michael Block (https://doi.org/10.1016/j.joms.2021.01.033) suggests that implant failures are more common among patients who have previously had COVID-19 and are more common soon after developing COVID.
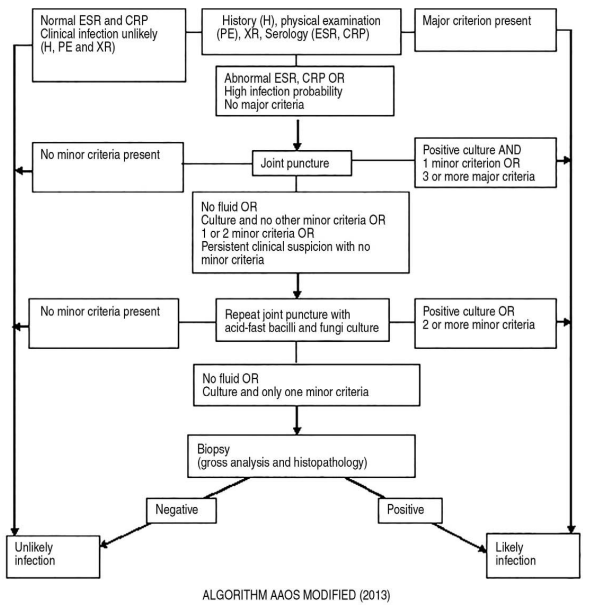
Diagnostic testing[edit]
The flowchart below shows one algorithm for diagnosing a periprosthetic joint infection (periprosthetic = close to prosthetic). Testing includes:
- May include symptoms such as:
- Pain/redness/warmth/drainage at the incision site
- Swelling of the joint/limb
- Pain or stiffness in the joint after a pain-free period
- Fever
- Chills or night sweats
- Fatigue
- General malaise (a general feeling of discomfort, illness, or uneasiness whose exact cause is difficult to identify)
- Blood tests to measure ESR (Erythrocyte sedimentation rate) and CRP (C-Reactive Protein). Both are associated with inflammation generated by infections.
- Fluid samples from the joint. These samples can be cultured to look for bacteria and fungus/yeast. However, many potentially pathogenic microorganisms are difficult to culture so these tests may yield false negatives. Culture-negative PJI (Periprosthetic joint infection) has been reported in 7% of PJI episodes treated at Mayo Clinic Rochester from 1990-1999 (see https://doi.org/10.1086/522184). The Lee and colleague study for breast implants suggests that periprosthetic joint infection may be heavily underdiagnosed if only 7% of PJI treated episodes are culture-negative versus >60% in breast implant illness.
- Biopsy
Source: Figure 1 from https://dx.doi.org/10.5371%2Fhp.2021.33.1.11
Other tests include:
- Elevated white blood cell count in synovial fluid (the fluid that lubricates joints).
- Elevated neutrophil percentage in synovial fluid.
- Purulence (pus) in the affected joint.
- Nuclear imaging
- D-dimer, which has limited performance for the diagnosis of joint infection. It has a false negative rate of around 18% and false positive rate of around 30% (https://doi.org/10.1186/s13018-020-01761-z).
References:
- Current Guideline for Diagnosis of Periprosthetic Joint Infection: A Review Article https://dx.doi.org/10.5371%2Fhp.2021.33.1.11
- Periprosthetic joint infection: Current concept https://dx.doi.org/10.4103%2F0019-5413.106884
Treatment[edit]
Unfortunately, pathogens growing in biofilms are extremely difficult to eradicate with antibiotics/antifungals and are resistant to eradication by the immune system.
Removal of the medical device or prosthetic can eliminate the environment that helps biofilms thrive. However, certain types of explantation surgeries (e.g. pacemakers, heart valves) are very risky.
Antibiotics and antifungals are often prescribed to people with replacement joint infections. However, it is known that bacterial and fungal biofilms are highly resistant to antibiotics and antifungals.
The chronic Lyme / PTLDS literature may offer some hope for non-surgical treatments. Animal model experiments by Monica Embers and colleagues provide strong evidence that Borrelia bacteria biofilms can cause chronic illness (see https://youtu.be/kZyI46hRIrk and https://doi.org/10.3389/fmed.2021.666554). Anna Goc and colleagues have found that chemicals produced by plants are effective in dismantling biofilms in lab environments as well as in human beings. A non-controlled trial on humans (https://doi.org/10.1177/2040622320922005) found that 3/17 participants became symptom free and an additional 8/17 participants demonstrated significant improvement. Feng, Zhang, and colleagues have also found that the drug combination Daptomycin + Cefoperazone (or Cefuroxime) + Doxycycline is effective in fighting Borrelia bacteria biofilms (see https://doi.org/10.1371/journal.pone.0117207 and this paper); there are currently no human studies reporting on how well this drug combination works in real world settings. Wang and colleagues (https://doi.org/10.1038/s41598-022-08948-w) tested tranexamic acid on mice and suggest that tranexamic acid "protects against implant-associated infection by reducing biofilm formation in infected tissues".
Total joint replacements and blood clotting syndromes[edit]
Warkentin and Greinacher (https://doi.org/10.1016/j.thromres.2021.05.018) argue that knee replacement leads to a blood-clotting syndrome (spontaneous heparin-induced thrombocytopenia or HIT) that is very similar to vaccine-induced immune thrombotic thrombocytopenia. Whereas HIT can develop following exposure to heparin, the authors believe that HIT can develop without exposure to heparin. They refer to that form of HIT as spontaneous HIT. However, the authors do not point out a common mechanism between vaccination and knee replacement surgery that would explain why the body usually (but not always) produces auto-antibodies against PF4. They believe that "further clinical and laboratory data will be needed" to determine the drivers of VITT.
The authors note that spontaneous HIT is more common after knee replacement than hip replacement. Warkentin and Cuker have since published a Feb 2023 review on VITT (COVID-19: Vaccine-induced immune thrombotic thrombocytopenia (VITT)) which discusses various mechanisms of action.
Essure (permanent birth control for females)[edit]
Essure injuries and Facebook support group participants were featured in the Netflix documentary The Cutting Edge.
Symptom prevalence reported in a paper by Maassen and colleagues (https://sci-hub.se/https://doi.org/10.1016/j.jmig.2018.10.009) are as follows:
| Symptom | Prevalence (%) |
|---|---|
| Abdominal pain | 69.9% |
| Back pain | 31.2% |
| Fatigue | 31.2% |
| Pain in legs and hips | 29.0% |
| Dysmenorrhea (severe and frequent menstrual cramps and pain during a woman's period) | 18.3% |
| Heavy menstrual bleeding | 17.2% |
| Skin rash | 16.1% |
| Cycle changes | 15.1% |
| Pain in joints | 11.8% |
| Intermenstrual bleeding | 9.7% |
| Dyspareunia (persistent or recurrent genital pain that occurs just before, during or after intercourse) | 9.7% |
| Itching | 8.6% |
Some symptom frequencies are similar to long haul while others are not (e.g. intercourse-related pain, rash, pain in legs and hips, back pain, abdominal pain).
A paper by Clark and colleagues (https://doi.org/10.1016/j.jmig.2017.05.015) found that perhaps 31% of patients had ongoing or worse symptoms after Essure removal. They recommend that patients "be counseled that some symptoms may persist or even worsen following surgery".
Surgical mesh implants[edit]
A case series by Jan Tervaert (doi:10.1016/j.berh.2019.01.003) described the development of ASIA syndrome (autoinflammatory/autoimmunity syndrome induced by adjuvants) following polypropylene mesh implantation, commonly used in hernia repair and pelvic organ prolapse surgery. Of the 19 patients who underwent surgery to try to remove the mesh, complete mesh removal was possible in only six patients. This resulted in "(partial) recovery of the systemic disease".
2 patients seen by the clinic committed suicide as they "had severe weight loss with abdominal pain that was considered by them to be not bearable resulting in suicide".
A listing of mesh support groups can be found on the website The Flower Empowered: https://theflowerempowered.com/pelvic-mesh-support/
Prevalence[edit]
A poll in a neurological vaccine injury support group (Facebook) found that 51/207 respondents (24.6%) had a medical device (e.g. breast implant, IUD, mesh, clamps) inside them.
The roughly one-in-four prevalence may be higher than the general population:
- Of women aged 15-49 years, 6.1% of North American women and 17.1% of European women use IUCs (intrauterine contraception). Source: Buhling and colleagues (https://doi.org/10.1016/j.contraception.2013.11.011).
- According to Cook and Perkins (https://doi.org/10.1007/978-3-642-85226-8_45), roughly 0.808% of women report ever having had some type of breast implant.
- "The 2010 prevalence of total hip and total knee replacement in the total U.S. population was 0.83% and 1.52%, respectively." Source: https://dx.doi.org/10.2106%2FJBJS.N.01141